Erin_Thibert
My Public Health Training

My Diagnosis
During the Advanced Medical & Public Health Internship, I had the opportunity to collaborate with medical professionals from around the world and gain hands-on experience in patient evaluation and diagnosis.
Using telehealth technology, I connected with a hospital in Bauchi State, Nigeria, where I engaged in real-time consultations with patients. Under the guidance of a Nigerian physician, I applied my training to diagnose and address some of the country’s most pressing health issues.
The patients I worked with were living on less than $1.25 a day without access to consistent medical care. Their participation not only gave us the chance to apply our training in real-world settings, but it also allowed them to receive fully funded treatment through Leadership Initiatives, providing critical care that would otherwise be out of reach.
This partnership model helps bridge global health gaps, ensuring that education and impact go hand in hand.
My Public Health Presentation
At the conclusion of the program, I had the opportunity to present my public health campaign to a panel of experienced doctors and public health professionals. The campaign I developed focused on increasing awareness and prevention of ARIs, a major health concern in the region. After a thorough review, the panel approved the campaign for official implementation in communities across Bauchi, Nigeria.
The campaign is designed to educate community members on practical, accessible prevention strategies that can be implemented in daily life. By focusing on education and prevention, the campaign aims to reduce the incidence of ARIs, improve early detection, and empower individuals to take control of their health.

My Public Health Campaign
I had the opportunity to learn about four of the most critical diseases in the developing world from esteemed medical professionals, Dr. Zainab Ibrahim, Dr. Aminu Yusuf, and Dr. Aishatu Nalado, from the Kano Teaching Hospital.
With their guidance, I gained a deeper understanding of the signs and symptoms of malaria, typhoid fever, acute respiratory infections (ARIs), and nutritional anemia, including how these diseases present at different stages. I also developed cultural competency and a global perspective, allowing me to examine the social and structural factors that contribute to poor health outcomes in underserved regions.
Collaborating directly with international development and public health experts, I helped create an impactful educational campaign tailored to the needs of underserved communities in Bauchi. The campaign focused on ARIs and promoting positive behavioral changes. Throughout the internship, I engaged in rigorous research and analysis to ensure the campaign was effective and relevant to the local population.
The process of developing the public health campaign was both challenging and rewarding. I conducted in-depth research on prevalent health concerns in the Birshi Gandu and Sabon Layi communities, identifying key areas where intervention and awareness were essential for improving health outcomes. Working with mentors and fellow interns, I formulated innovative strategies to engage the community and ensure the campaign’s messages resonated with the intended audience.
Clinical Skills Training

Phlebotomy
As part of my clinical training, I practiced phlebotomy using an anatomical arm model designed to simulate realistic vein-wall resistance.
With guidance from a medical facilitator, I refined my technique and improved my communication skills, helping me prepare to interact with future patients.

Laparoscopy
I studied laparoscopy, a minimally invasive surgical technique that allows physicians to examine and treat internal organs using small incisions and specialized, camera-guided instruments.
After learning how the technology works, I had the opportunity to perform a simulated laparoscopy, applying my knowledge and gaining insight into this surgical method.

Intubation
Under the instruction of EMTs, I learned various emergency resuscitation techniques, including manual esophageal intubation and the use of resuscitation airway masks to maintain the airway.
The EMTs provided hands-on instruction on when to apply different airway management methods and how to choose the correct equipment in emergency scenarios. This training gave me a strong foundation in life-saving procedures.
Internship Highlights

During this internship, I had the incredible opportunity to learn from leading professionals in surgery, emergency medicine, neuroscience, public health, and medical research.
One of the highlights was a session with Dr. James Giordano, Chief of Georgetown University’s Neuroethics Studies Program, whose insights deepened my appreciation for the ethical challenges and advances in neuroscience. I also engaged with experts from the D.C. Department of Health and Human Services, active EMTs, global health leaders, and physicians from Children’s National Hospital.
These experiences gave me a well-rounded understanding of the day-to-day responsibilities within various medical fields and offered valuable guidance on the educational paths and skills needed to pursue careers in healthcare.

Under the mentorship of Dr. Zainab Ibrahin, Dr. Aminu Yusuf, and Dr. Aishatu Nalado, I developed essential skills in patient interviewing and disease investigation.
Throughout the program, I honed my abilities in collecting, interpreting, and critically analyzing patient data. Their guidance significantly enhanced my capacity to synthesize and evaluate information, which is crucial for the diagnostic process. These exercises also improved my communication skills for effective patient evaluation.
Additionally, their expertise provided me with a comprehensive understanding of current practices in Nigerian medicine. Meeting and learning from real patients gave me a deep appreciation for the lived experiences of individuals in Nigeria, influencing my perspective on implementing effective strategies in my campaign to combat infectious diseases.

Throughout the internship, I had the invaluable opportunity to build essential clinical skills that strengthened my understanding of patient care. Among the techniques I learned were taking vital signs and performing comprehensive neurological exams.
With guidance from experienced mentors, I practiced various methods for measuring a patient’s pulse and accurately calculating heart rates across different age groups and health conditions. This hands-on training gave me the confidence to assess patients effectively and respond to their needs with greater precision.
Learning to take vital signs and conduct neurological assessments is a critical step in ensuring patients receive timely and appropriate care, as these skills form the foundation for effective diagnosis and treatment.
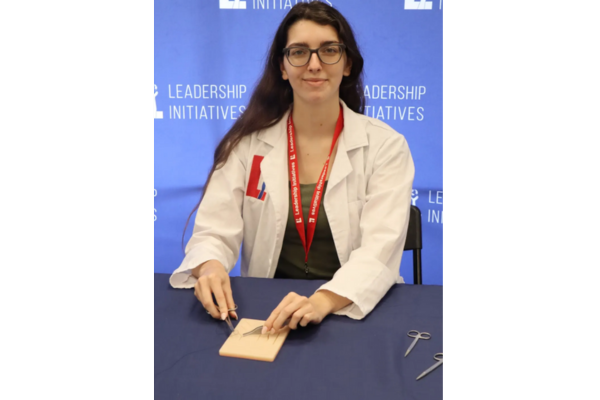
One of the most hands-on experiences during the internship was learning and practicing multiple suturing techniques using a human skin model.
I explored the purpose and application of different suturing methods across various clinical scenarios. This training gave me a deeper appreciation for the precision and care required in wound management, and it highlighted suturing as a vital skill in both emergency and routine patient care.
In addition to suturing, I also learned how to apply plaster casts, further expanding my exposure to essential medical procedures. These hands-on activities helped me better understand the diverse skills healthcare providers use daily to care for patients and respond to medical needs.